Other than taxes, the only other certainty in life is death. People don’t like to pay taxes or think about dying. But on April 16th, National Healthcare Decisions Day (NHDD) reminds people to complete their advance directives. Like a passport, an advance directive permits an individual to proceed from one world to another with an easy stamp of approval. Without the proper paperwork, patients at the end of life are often detained and experience loss of dignity. Instead of being a natural process, dying has evolved into a medicolegal nightmare with only a DIY option for ethical end-of-life care.
If a 93-year-old woman in a diaper presents to the emergency department in extremis, is it more respectful to shove a breathing tube into her lungs or provide her comfort care? Does she have an advance directive and what does it state? What does her family advocate? Should this be anyone’s guess or can medical personnel follow a standard emergency protocol? This woman’s medical condition is life-threatening and prognosis is futile. It’s unlikely that she wishes for aggressive treatment given her limited quality of life. Might the treating physician do unto her as he would prefer others do unto him without questioning if she has an advance directive?
Who ultimately ensure the dignity of this woman and decides the moral course of action?
When natural disaster occurs, we follow a basic plan of action while awaiting further instruction. When a life-threatening event such as difficulty breathing or cardiac arrest occurs, 911 is called or the “Code Blue” is enacted. The normal course of action is to start CPR, but are further instructions provided? Two out of three people haven’t formulated or completed their advance directives. This means there’s no personal disaster plan (advance care plan) or manual (advance directive).
NHDD serves as a reminder that D-day or personal disaster day requires a decision plan for whether to provide medical intervention or end-of-life care. Yet, most people cannot imagine having a heart attack, brain damage, terminal cancer, or being burned beyond recognition. They’re at a loss for words in these moments and need both an advance directive and healthcare proxy/medical power of attorney who can speak for them. Yet, this abdication of duty persists.
A code blue is relatively common in the emergency department and personnel start Advance Cardiac Life Support (ACLS) as per standard healthcare protocol with no questions asked. Most EM physicians don’t consider advance directives helpful because patients are not usually transported to the ED for end-of-life care. And it’s presumed that family caregivers want life-threatening conditions reversed. Family members often claim: “I’m not ready” to make the tough decision that permit death.
The following Advance Directive Decision-Tree for Caregivers (ADDT) offers a brilliant algorithm for any doomsday scenario.
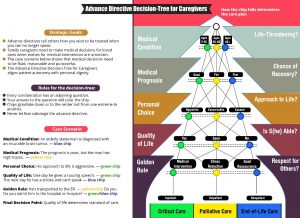
Imagine a world without fear of dying. Imagine a world where the dying are cared for without family members needing to say anything or feel negligent by not advocating for critical care. Advance directives play off an individual’s fear that others might either attempt to hasten death or prolong life. This infographic provides both patient and caregiver a template by which to put their fear to rest and establishes guiding principles for all first responders.
Standardized care is the best practice of medicine and the ADDT needs to replace individual advance directives. Even if these personal documents are readily available, they rarely address the medical situation at hand and patients are likely to change final wishes as medical conditions worsen. With any natural disaster, authorities are not obliged to ask the public what their wishes are. Public authorities conduct training programs and disaster drills. This way everyone know what’s expected of them and how to act responsibly. ADDT is an easy-to-follow template that guides healthcare decisions and allows family members and healthcare providers to ”think, say and do” from one advance directive.
National Healthcare Decisions Day encourages advance care planning to ensure all people die with dignity. It might better serve society through promoting and educating them about the Advance Directive Decision-Tree for Caregivers. When this protocol is understood and adopted as the best practice of medicine, a good death might be possible for everyone on any given day.
Leave a Reply